Alternative health practitioners support their clients’ health through a combination of nutritional and lifestyle changes, while conventional medicine practitioners typically use drug-based approaches to reverse or mask symptoms of diseases.
Traditionally they have viewed health and disease very differently.
Things are changing however, and with it comes the emergence of Lifestyle Medicine.
In this article we’ll take a closer look at Lifestyle Medicine and how it may revolutionise healthcare of the future.
Genetic discoveries
In an ambitious project which ran from 1990 to 2003, scientists determined the DNA sequence of the entire human genome.
The expectation was that this study would provide clear information about the crucial role our genes play in health.
Previously it was believed our genes were more or less fixed, determining whether or not a particular disease developed.
In fact, the project told us something very different: genes could be switched on or off by environmental factors.
This means our environment determines whether genetic tendencies are expressed into factors which lead to the development of a disease.
It was discovered that only 10% of disease risk is down to genetics, the other 90% is down to environment.
So what is of overriding importance is not so much our genes – although these can provide clues about susceptibility – but our environment.
Lifestyle diseases
The role of the environment becomes more obvious when we think about the huge rise in lifestyle diseases over the past decades.
According to the NHS, hospital admissions in which obesity played a role increased by 18% in just one year between 2016 and 2017, while over 62% of adults in the UK are now classified as obese or overweight.
Type 2 diabetes, another lifestyle disease, has increased from 1.4 million in 1996 to 3.5 million today.
If the present growth continues, it’s estimated it will affect 5 million people in the UK by 2025 (1).
It’s impossible our genetics could have changed so rapidly, so it must be the environment playing the major role.
According to the World Health Organization, non-communicable chronic diseases are the leading cause of death worldwide, responsible for 71% of these deaths in 2012, many of them premature.
Research looked at four lifestyle factors: stopping smoking, increasing exercise, following healthy eating advice and having a BMI of less than 30.
Scientists concluded changing these four factors could prevent as much as 93% of cases of diabetes, over 80% of heart attacks, half of all strokes and 36% of all cancers (2).
Environment
Many factors make up your environment, including:
- Nutrition, including alcohol consumption
- Stress levels
- Pollution, including smoking
- Movement and exercise
- Sleep
A huge amount of research is being carried out on all these factors, and fascinating discoveries are being made every day about their effects.
It’s becoming clear the environment can influence health in many ways, even down to affecting the behaviour of the molecules in your cells.
Lifestyle Medicine
All this emerging research has resulted in many medical practitioners moving towards an approach which recognises the importance of the effect environment has on health.
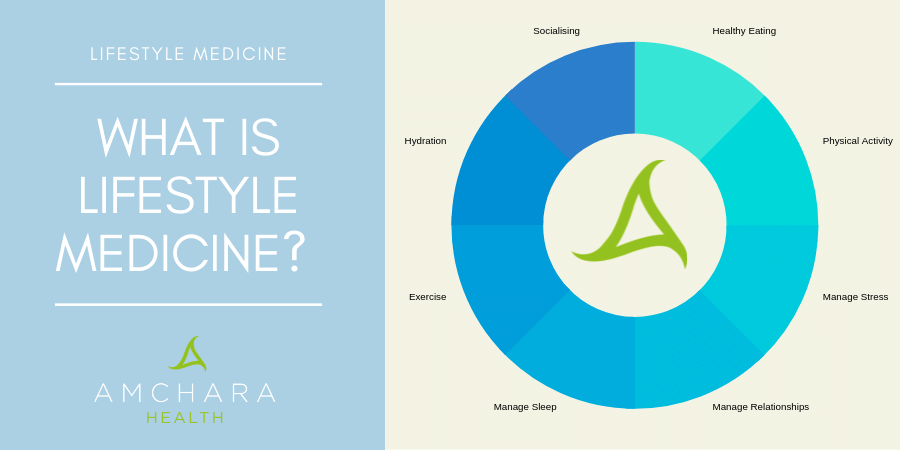
Lifestyle Medicine is defined as a medical speciality using the latest evidence to prevent or treat chronic disease by the modification of sustainable lifestyle factors.
To practise Lifestyle Medicine, GPs need an understanding of how environmental, social and emotional factors contribute to ill health.
Advice includes recommendations to adopt whole food, plant-based eating, move regularly, manage stress and avoid exposure to dangerous substances such as chemicals.
Lifestyle modifications are generally low cost or free, safe and relatively easy to make, and they empower the patient to take control of their own health.
Critics say this shifts the blame for ill health onto the patient, which highlights the importance of a good patient/GP relationship, with advice being delivered with sensitivity.
The skill in imparting lifestyle advice for GPs will be to encourage behavioural change so the lifestyle changes are sustainable.
The GP is in a strong position to change patient behaviour through their recommendations, because they are seen as experts by patients.
One problem with Lifestyle Medicine is that GPs may have trouble fitting truly personalised lifestyle recommendations into a short consultation.
More emphasis on prevention
Lifestyle Medicine is about the prevention, as well as the treatment, of lifestyle diseases, and aims to increase healthy longevity.
It does require the patient to be seen as a whole rather than simply a collection of symptoms, something which has always been at the heart of the philosophy of natural health practitioners.
Lifestyle Medicine is being introduced into the curriculum at some medical hospitals, but doctors still remain poorly trained in nutrition, receiving an average of only 20 hours training on nutrition over their entire medical course (3).
Lifestyle Medicine and Personalised Health
Here at Amchara Personalised Health is at the heart of what we do.
A consultation with a Personalised Health practitioner recognises your biochemical individuality, as well as the importance of the environment in determining whether your genetic tendencies are expressed.
Practitioners study the latest research to ensure their therapies are evidence-based.
Functional tests are used to detect imbalances in the body and discover the root causes of disease.
If all this sounds not too dissimilar to the concept of Lifestyle Medicine, then you are not mistaken.
The major difference is that typically a consultation with a Personalised Health practitioner would last at least an hour, whereas the average GP consultation in the UK is just under ten minutes.
This obviously enables a far more in depth case history to be taken, so the underlying causes of ill health can be better identified.
It also means dietary and lifestyle recommendations can be completely personalised.
Takeaway
A consultation with a Personalised Health practitioner can help you identify not only your own genetic picture, but lifestyle factors which can support or hinder the expression of your genes.
We’re dedicated to providing you with both insightful information and evidence-based content, all orientated towards the Personalised Health approach.
Did you find this article useful?
What do you think about Lifestyle Medicine?
We would love to know your thoughts.
READ THIS NEXT: