The Digestive System | What can go wrong? | Problems | Solutions | Treatments | Free Gut Health Consultation
“All Disease Begins in The Gut.” – Hippocrates
It seems like every week new studies and headlines are pointing towards gut health as being the cornerstone for healing conditions or reaching optimum wellness.
From IBS to complex autoimmune conditions improving your gut health can bring benefits to your whole body.
This isn’t actually a new idea, over 2000 years ago Hippocrates said ‘all disease begins in the gut’ and research in more recent times has confirmed he was definitely on to something!
Understanding how your body works is often the first step towards making the changes needed to make sure you inhabit a healthy body that’s disease free…
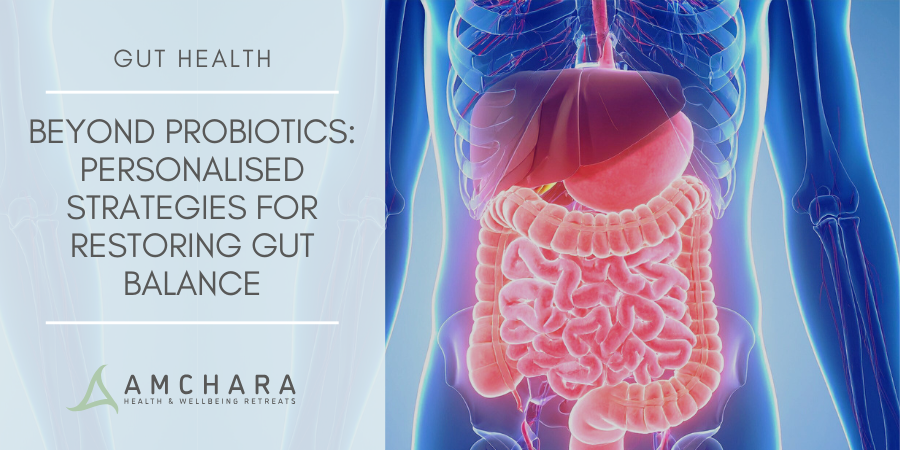
The Mysteries of Your Digestive System
Your digestive system is an amazingly complex mechanism, responsible for absorbing and transporting every nutrient you ingest to ensure your body thrives – it also helps to rid your body of waste and protects you from unwanted gremlins!
Keeping your digestive system healthy and ticking over nicely is therefore essential to your future health and ability to prevent disease.
The Mouth
This is where it all starts…the minute you think about food, the sight and smell sends messages to your brain, prompting the digestive process by triggering salivation, which not only aids swallowing but also contains amylase an enzyme in your saliva that helps to digest the starchy parts of your meal.
The oesophagus (food pipe)
The food you have chewed slides down the oesophagus helped by peristalsis – a wave of muscle contractions – that propel it towards the stomach. A sphincter muscle at the end of the esophagus quickly opens and shuts to let the food into the stomach where it is greeted by a churning pool of digestive juices.
The stomach
Glands in the stomach secrete acid and protein-digesting enzymes, which break down the food as well as helping to kill bacteria.
The cells lining the stomach also produce thick mucus that coats the stomach protecting it from its own acid. Other specialised cells produce a special carrier that helps the body to absorb vitamin B12. The final soupy substance the stomach produces is called ‘chyme’.
The duodenum (small intestine)
The chyme is released gradually into the small intestine.
Once the food is recognised, the duodenum releases two hormones called secretin and cholecystokinin (CCK) which send messages to the brain, stomach, pancreas, and gallbladder, to indicate satiety and also to slow down the stomach emptying process and to release digestive juices.
Ducts from the liver, pancreas, and gallbladder, enter the duodenum to deliver juices that neutralize acids coming from the stomach and help digest proteins, carbohydrates, and fats.
There are a number of pancreatic enzymes at work these include:
- Trypsinogen – a precursor for the protein-digesting enzyme trypsin
- Chymotrypsinogen – a precursor for the protein-digesting enzyme chymotrypsin
- Lipase – a fat-digesting enzyme
- Pancreatic amylase – a carbohydrate-digesting enzyme
The process of peristalsis mixes the chyme up with digestive juices and pushes it further down the gut.
The Jejunum and Ileum
These last two sections of the small intestine finish the digestive process and also facilitate absorption of the digested nutrients and water.
The small intestine has an extremely large surface area due to the tightly folded layers of tissue, which are covered in finger-like projections called villi. The entire surface is replaced every three to five days.
After the final stages of digestion, the nutrients are released and absorbed into the bloodstream where they are transported directly to the liver.
The liver being the largest organ in the body has a number of metabolic and secretory functions and decides which nutrients should be processed; whether they are stored, eliminated via the stool or sent back into the general circulation.
The large intestine
Following absorption of all the important and beneficial parts of your food, the remaining parts that are indigestible are transported into the large intestine to be prepared for elimination.
The large intestine is composed of the caecum and also the colon, which is divided into the ascending colon, the transverse colon, and the descending colon.
The ascending and transverse colon are responsible for absorbing salts and extra fluid and producing mucus to make sure there is a properly formed stool that is passed easily.
The rectum is the final section of the large intestine where the stool sits waiting to be excreted through the anus.
What can go wrong?
As we’ve seen the first part of the digestive process starts in the mouth.
Chewing is vital to ensure that food is adequately mixed with saliva and sufficiently broken down.
Eating too quickly means that the stomach receives food before the acid and protein digesting enzymes are ready to do their work.
Partially digested proteins can then make their way through the rest of the digestive tract, which may create absorption problems and inflammatory issues.
Imbalances in stomach acid production can create problems.
The correct balance of stomach acid is central to a healthy digestive system, but in some cases, individuals can produce too much or too little.
Excess stomach acid can irritate the stomach lining causing pain and may even lead to stomach ulcers.
An ulcer is essentially a hole in the lining of the digestive tract, most commonly in the oesophagus, stomach and duodenum.
There are a number of factors that can trigger excess stomach acid production:
- Alcohol
- Smoking
- Coffee
- Red meat
- Aspirin
- Fizzy drinks
- Wheat
- Spicy foods
- Fried foods
- Garlic
- Onions
An H. pylori (Helicobacter pylori) infection can also lead to ulcers.
An overgrowth of this particular pathogenic bacterium weakens the protective mucus in the stomach and in some cases increases gastric acid secretion allowing acid to eat through. Research shows that over 90% of duodenal ulcers and 70% of gastric ulcer patients are infected with H. pylori.
Certain medications such as NSAIDS (non-steroidal anti-inflammatories) also inhibit mucus secretion inducing gastric damage.
Low stomach acid can be equally problematic.
Insufficient gastric acid prevents food from being fully broken down because the acid is needed to convert pepsinogen to pepsin, an enzyme that initiates the digestion of protein.
This means that some proteins and nutrients are unprepared for absorption. Stomach acid also plays a key role in eliminating bacteria, so low levels can leave you susceptible to digestive infections.
A number of studies have identified that stomach acid secretion declines with age particularly amongst those over 60. Further research has also shown that 40% of postmenopausal women have no basal gastric acid secretions.
Another contributing factor in low stomach acid is vitamin and mineral deficiencies.
Zinc, in particular, is a mineral that is necessary for gastric acid production. Chronic stress can also impair the body’s ability to produce sufficient gastric acid.
Loss of tone or function in the lower esophageal sphincter may lead to heartburn.
If the sphincter (the ring of muscle that acts as a seal on top of the stomach) doesn’t close properly stomach acid can splash into the esophagus causing heartburn. However certain foods such as peppermint and chocolate can also cause the sphincter to relax more than normal.
Delays in the secretion of bile and pancreatic juices can lead to compromised digestion in the small intestine and subsequently problems with the absorption of nutrients.
Often this is due to poor digestion in the stomach which delays food entry into the duodenum. Even with a healthy diet, this could result in nutrient deficiencies.
Food intolerances can also occur as a result of adverse reactions to a food, usually caused by an inability to digest or absorb certain foods. A good example of this is lactose intolerance.
Up to 70% of the world’s population cannot produce the enzyme lactase, which aids the digestion of lactose – the sugar found in milk. Undigested lactose sits in the intestine and ferments, causing bloating, abdominal pain, wind and diarrhea.
Foods most often linked to intolerances include dairy products, grains that contain gluten, and poorly absorbed sugars that cause a build-up of gas in the intestines such as FODMAPS (fermentable oligosaccharides, disaccharides, monosaccharide’s and polyols).
Some examples of FODMAPS include:
- Garlic
- Leek
- Onions
- Milk
- Beans
- Lentils
- Many fruits
- Chickpeas
- Asparagus
- Artichoke
- Barley
- Rye
- Wheat
A lack of fibre in the diet can affect the ease and frequency of bowel movements.
Fibre is needed to soften and bulk out the stool and helps to trigger the muscular movements that propel waste through the colon.
A diet that is lacking in fruit and vegetables and high in refined and processed foods can result in constipation and in the long term may lead to haemorrhoids (piles).
In addition to this, infrequent bowel movements can mean that waste matter sits in the large intestine; putrefying and fermenting, which can lead to bloating, wind and discomfort.
Waste products destined for elimination can also be re-absorbed into the blood circulation increasing toxins and placing an additional burden on the liver.
People with chronic constipation often complain of fatigue and skin problems.
How do you know if you have a problem?
Many people will experience symptoms of digestive discomfort at some point in their lives and often this passes, but when the symptoms start to dominate your life it can be a sign of poor gut health.
Some common symptoms include:
- Bloating
- Stomach cramps
- Fatigue
- Reactions to foods
- Irregular bowel movements
- Flatulence
- Diarrhoea
- Constipation
- Nausea
Digestive issues can also manifest in skin conditions, autoimmune illnesses and depression.
Over 70% of your immune system is located in your digestive tract so the implications of good gut health can be incredibly beneficial for all-round health and well being.
Be good to your gut
So if good gut health is so important what can you do to support your digestive system?
There are a few important steps to take:
- Chew your food properly – don’t hurry your meals, slow down and give your brain time to register that food is arriving in the stomach so that it can stimulate the release of stomach acid.
- Eat a balanced diet to gain a good range of nutrients. Make sure your meals include plenty of fruit and vegetables, whole grains, good quality protein and healthy fats. Try to avoid highly processed sugary foods, alcohol, and caffeine.
- Support your gut flora by encouraging healthy bacteria to flourish. Good bacteria help to keep pathogenic bacteria from proliferating.
- They ferment fibrous foods to special substances known as ‘organic acids’ that stimulate the growth of the gut lining.
- The gut lining is very delicate and can be easily damaged by poorly digested foods and toxins. A more permeable or ‘leaky’ gut barrier can allow large protein molecules and toxins to pass into the bloodstream causing systemic inflammation throughout the body. Leaky gut is prevalent in modern society mainly due to stress, poor dietary choices and environmental toxins.
- Counteract oxidative damage by making sure your diet is rich in antioxidants.
- The gut lining is extremely delicate and easily damaged not just by undigested food particles but also by free-radical molecules that are unstable, highly reactive and capable of causing considerable oxidative damage.
- Antioxidants are the first line of defence against free radicals and environmental toxins, so a well-designed antioxidant programme can do wonders for maintaining a healthy gut.
- The optimum antioxidant programme should include co-enzyme Q10, vitamins C,D,E and the B group, a range of carotenoids plus flavonoids and the full range of antioxidant trace metals.
- Topping up on these important antioxidants is made easier if you eat plenty of fruit and vegetables. Plant foods are the best sources of antioxidants, not only can they survive cooking to be absorbed by the body but they also contain compounds which stimulate the production of the body’s own antioxidants and detoxifying enzymes plus other compounds that benefit gut health.
Give your gut a break
One of the best ways to repair the gut barrier is to rest the digestive system by fasting.
This allows the body to carry out essential repair work on a cellular level, restoring the lining and reducing permeability.
This break also de-stresses the system and can assist in weight loss, as the body will switch to using your natural energy reserves.
Fasting doesn’t necessarily mean starving for days at a time, recent scientific evidence shows that there are many ways of fasting that still provide numerous health and weight loss benefits normally associated with restricting food intake.
Intermittent fasting is one of the more popular fasting methods and is a great way to reap the benefits of much stricter water fasting and work it into your everyday life.
You could follow the popular 5:2 method or do a daily 16-hour fast (mainly when you are asleep!) with an 8-hour eating window.
You might also consider trying the fast mimicking diet – a really effective five-day method that you can follow once a month.
It’s about finding what works for you.
Nourish your gut
Good gut flora is integral to good gut health, without a doubt, the two are closely linked – if you have leaky gut chances are you will also have poor gut bacteria.
Why is this important?
The body contains 10 times more bacteria than all the human cells in the entire body roughly 2kg are thriving in your gut!
The bacteria in your gut are essential for assisting with digestion and optimum absorption of nutrients so it is essential to have a well-balanced gut flora.
Removing sugar, processed foods, common allergens such as gluten and dairy as well as adding in fibre rich and nutrient dense vegetables and fermented foods will all contribute to a rich and varied gut flora.
Supplementing with a probiotic (friendly bacteria) will further bolster your efforts and a diet rich in pre-biotic foods such as onions, garlic, and Jerusalem artichokes will ensure your good bacteria have a nutrient source.
Healthy gut, healthy body
Improving gut health is a great starting point for addressing many common health conditions and symptoms and is an integral part of working to improve overall health and well-being.
A functional approach to treatment that considers the body as a whole can support your journey to optimum wellness. Making good nutritional choices, reducing stress and toxins and supporting healthy bacteria to flourish will help to heal the gut barrier and prevent many common digestive issues.
Related Gut Health Topics:
- Common Gut Problems
- Is My Gut in Balance?
- Leaky Gut and Grains (and why to avoid them)
- The Gut at the Centre of your Health
- Good Health Starts in the Gut
- New Study Shows a Gluten Free Diet Influences Gut Health
- Fasting For Gut Health
- Antibiotics and Gut Health
- Control IBS With These 7 Foods
- Is IBS making you miserable?
Sources
- Arebi N et al. How does Helicobacter pylori cause mucosal damage? It’s effect on acid and gastrin physiology.Gastroenterology. 1997;113(6 Suppl):S43-9.
- Barrett JS & Gibson PR. Fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) and nonallergic food intolerance: FODMAPs or food chemicals? Therap Adv Gastroenterol. 2012 Jul; 5(4): 261–268.
- Chandra N, Lobo V, Patil A & Phatak A. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn Rev. 2010; 4(8): 118–126.
- Gillen D, McColl KEL & Omar EE. Interactions between H. pylori infection, gastric acid secretion and anti-secretory therapy. British Medical Bulletin 1998;54 (No. 1): 121-138.
- Healthy Eating Advisory Service. Food intolerance. [Accessed 7.8.18.]
- https://www.britannica.com/science/small-intestine [Accessed 5.8.18].
- Hyodo I et al. The pathophysiology of non-steroidal anti-inflammatory drug (NSAID)-induced mucosal injuries in stomach and small intestine. J Clin Biochem Nutr. 2011 Mar; 48(2): 107–111.
- NUTRITION REVIEW. Gastric Balance: Heartburn not always caused by excess acid. [Accessed 6.8.18.]
- O’Connor HJ. The role of Helicobacter pylori in peptic ulcer disease. Scand J Gastroenterol Suppl. 1994;201:11-5.