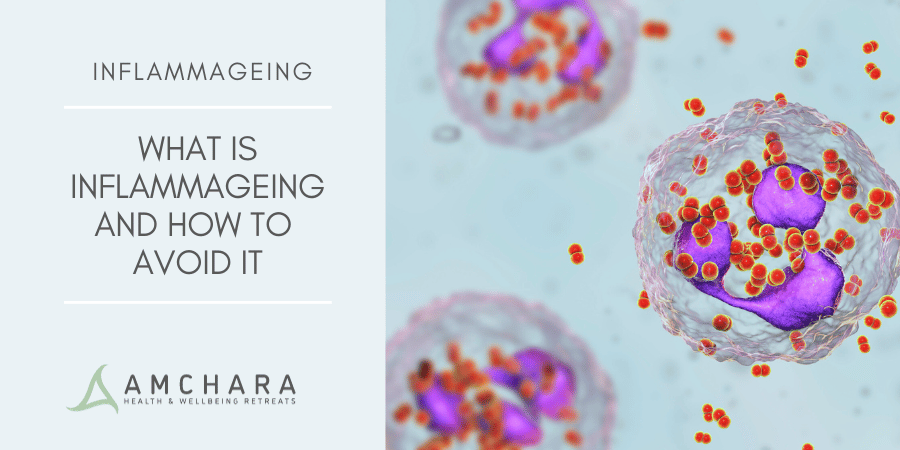
Metainflammation is the term used to describe the chronic, low-grade inflammation that is associated with metabolic dysfunction.
Unlike acute inflammation, which is a protective, and often localised, response to injury or infection, metainflammation is a systemic condition that may initially be asymptomatic, but unless addressed can lead to significant health issues over time.
In the modern internet world there is an overwhelming amount of information; it can be hard to find health advice that you can trust, particularly as the main media channels are typically dominated with a single, orthodox narrative.
Our articles are always evidence-based and oriented to a Personalised Health approach, and we aim to provide you with actionable knowledge and tips to help you on your journey to optimal health.
In this article we’ll look at which factors impact inflammation levels, what risks are associated with sustained, high levels of systemic inflammation, and why this is particularly important during and after menopause.
We will also offer some strategies to help you reduce inflammation and avoid the health outcomes associated with metainflammation.
What causes metainflammation?
Metainflammation is driven by the immune system’s response to excess nutrients and metabolic stress.
The inflammatory process is controlled by cytokines – proteins used by the body to regulate inflammation. These can be pro-inflammatory, used by the body in to trigger necessary inflammation and stimulate an immune response, or anti-inflammatory, used to suppress immune or inflammatory responses, or to heal an injury.
Problems arise when pro-inflammatory cytokines are continuously released, in response to lifestyle, dietary and environmental stressors.
This type of inflammatory state is linked to the development of various chronic diseases, such as obesity, type 2 diabetes, cardiovascular diseases, and even certain cancers.
What contributes to metainflammation?
Metainflammation is primarily influenced by modifiable lifestyle factors, particularly diet, physical activity levels, and exposure to pollutants.
The overconsumption of high-calorie, nutrient-poor processed foods, especially those rich in sugars and unhealthy fats, places the body in a state of chronic, low-level stress.
Not only do these foods contribute to fat storage and weight gain, which increases inflammation, they also lack the compensatory antioxidants and nutrients that whole foods provide.
Anti-inflammatory nutrients such as fibre, omega-3 fatty acids, and antioxidants, found in abundance in unprocessed, natural foods, can help to control inflammation in the body.
Incorporating more of these into your diet can help your body to deal with other factors that increase your inflammation levels.
In addition to diet, sedentary behaviour exacerbates metainflammation. Physical inactivity reduces muscle mass, impairing overall muscle metabolism. Muscle cells are much more metabolically active than fat cells, and help to control blood sugar levels.
A low muscle mass is therefore an important risk factor to consider, contributing to the development of insulin resistance, as well as decreasing your metabolic rate, and increasing the risk of inflammatory weight gain.
Moderate exercise has been shown to reduce levels of inflammatory cytokines, as well as promoting healthy circulation, and supporting the transport and elimination of waste products by the cardiovascular system.
Introducing more non-exercise related activity into your life, such as taking the stairs and walking rather than driving, can help to use and maintain your muscle mass.
However it is recommended that you spend at least 150 minutes a week participating in a form of moderate exercise. Weight training and other muscle-building activity can be especially useful in maintaining muscle mass, especially as you grow older.
Insulin resistance is another important contributing factor to the development of metainflammation, as elevated blood sugar levels stimulate the production of pro-inflammatory cytokines.
High blood sugar also damages the endothelium, or cell walls of the blood vessels, causing chronic inflammation in the cardiovascular system, as well as promoting fat storage.
Consumption of quick-release carbohydrates and sugar causes blood sugar to spike, and then drop dramatically, which can cause you to become stuck in a cycle of blood sugar highs and lows.
Frequent episodes of low blood sugar can also be inflammatory, triggering an adrenaline release and placing your body in a state of stress, as well triggering cravings for sugary foods, and impacting your ability to make heathy choices.
Reducing or eliminating refined sugar and carbohydrates, and ensuring that you consume adequate protein, fibre and healthy fats, alongside carbohydrate rich foods can help to balance blood sugar levels.
Pollutants and environmental toxins also contribute to metainflammation. Exposure to air pollution, for instance, has been linked to increased levels of systemic inflammation.
Pollutants can activate immune cells, an inflammatory process, as the body reacts as if responding to a pathogen. Whilst it can be hard to avoid pollution in our modern world, exercising in more natural environments, away from roads, can help to reduce your exposure.
Cosmetics and body care products, cleaning products, diet and water can also be potential sources of pollutants – invest in natural products for use on your body and in your home, as well as using a water filter.
The link with chronic disease
The link between metainflammation and chronic diseases is well documented. For instance, in obesity, the excessive accumulation of adipose tissue not only promotes inflammation but also disrupts the normal functioning of adipocytes (fat cells).
Cardiovascular diseases, particularly atherosclerosis, are intrinsically linked to metainflammation. The body uses cholesterol to repair damage to the cardiovascular system, and over time this can lead to the accumulation of plaques within the arteries, and eventually to heart attacks or strokes.
In addition, metainflammation is linked to hypertension, as inflammatory cytokines can induce changes in blood vessels that increase blood pressure.
Chronic inflammation is also implicated in the development of non-alcoholic fatty liver disease, a condition that often coexists with obesity and diabetes, and can progress to more severe liver diseases.
Inflammation levels also have an effect on mental health, with chronic inflammation linked to mood disorders, such as depression and anxiety.
Mental health significantly impacts health outcomes, influencing physical health, chronic disease progression, and overall wellbeing.
Poor mental health can exacerbate stressors, reduce immune function, and can impact the ability to make healthy choices or manage health conditions, as well as increasing the risk of alcohol, drug or food abuse.
Emerging research also suggests that inflammation may play a role in the development of certain cancers.
Chronic inflammation affects the function of every cell in the body, increasing the risk of genetic mutations and the proliferation of malignant cells. For example, obesity-related inflammation is associated with an increased risk of colorectal, breast, and liver cancers.
Inflammation and the menopause
During menopause, the decline in oestrogen levels plays a significant role in altering inflammatory processes in the body.
Oestrogen is important in modulating inflammation because it has anti-inflammatory properties, primarily working to reduce the production of pro-inflammatory cytokines, while also enhancing the production of anti-inflammatory cytokines.
Oestrogen also influences immune cell function, promoting the activity of regulatory T-cells that help control inflammatory responses.
This protective effect helps maintain a balance in immune responses, reducing the risk of chronic inflammation related conditions, such as cardiovascular disease and osteoporosis.
However, the natural decline in oestrogen during menopause can lead to increased inflammation, contributing to various age-related health issues, making it even more important to control inflammation levels.
This increase in inflammation is associated with several health issues commonly seen in postmenopausal women. For instance, the heightened inflammatory state can exacerbate the risk of developing cardiovascular diseases, such as atherosclerosis, as well as contribute to insulin resistance, which can lead to the development of type 2 diabetes.
Additionally, inflammation is implicated in the progression of osteoporosis, where bone reabsorption outpaces bone formation, leading to increased fracture risk.
Inflammation can exacerbate menopause symptoms and increase the risk of related health issues, such as joint pain, mood swings, and fatigue.
Elevated inflammatory markers may also worsen hot flushes, which can cause social anxiety, disrupt sleep and increase stress levels, creating an inflammatory
feedback loop.
Takeaway
Metainflammation represents an important link between lifestyle, environment, and health outcomes, making it a crucial area of study in understanding the modern epidemic of chronic diseases.
Addressing this issue requires a multifaceted approach, including dietary modifications, increased physical activity, and reducing exposure to environmental toxins.
Understanding which factors increase inflammation empowers you to make informed lifestyle choices that target the underlying mechanisms of metainflammation; reducing the stress on your bodily systems and improving overall health outcomes.
Recognising the impact of diet, stress, and physical inactivity can help you to incorporate healthier lifestyle choices into your daily life, such as a nutrient-rich diet, regular exercise, and effective stress management.
During menopause this is especially important, due to the changes in hormonal function and levels that increase inflammation levels, and positive lifestyle choices can help to reduce the symptoms of menopause.
If you would like to find out more about reducing your levels of inflammation, come to Amchara where our Personalised Health practitioners will support you, recommending positive, sustainable lifestyle choices tailored to your individual health circumstances and goals.
Our Amchara detox health retreats are designed to help you both physically and mentally, and you will be immersed in a supportive and nurturing environment, combining a Functional Medicine and naturopathy approach, that enables you to switch off, relax and kickstart your health journey, and Change for Good.