Topics Covered in this article:
According to the International Osteoporosis Foundation, osteoporosis affects approximately 75 million people in Europe, Japan and the USA.
One in three women over the age of 50 will experience fractures due to osteoporosis. This also applies to men over 50 albeit to a slightly lesser degree – one in five men will experience osteoporotic fractures. (1)
We always take an evidence-based approach and aim to provide you with actionable knowledge and tips to help you on your journey to optimal health. In this article we look at contributing factors to osteoporosis, as well as symptoms, and tips on how to build your bone strength.
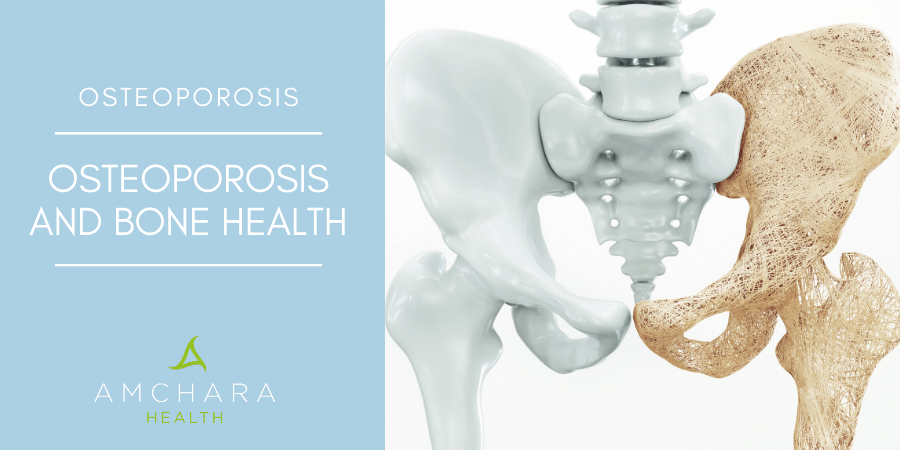
The term osteoporosis means ‘porous bones’. It’s a disorder of unbalanced bone remodelling, involving progressive deterioration of bone tissue, resulting in porous bones and ultimately a decrease in bone density, increasing the risk of bone fractures.
The whole skeleton can be affected by osteoporosis, however bone loss is generally greater in the hips, spine and wrists, where fractures commonly occur.
#1. Contributing factors
Osteoporosis can occur due to age, genetics, dietary intake and lifestyle factors. The causes are complex and include:
- Early menopause
- Irregular periods
- Family history
- Early hysterectomy
- Anorexia or bulimia
- Female hormone imbalance
- Small frame
- Smoking
- Excessive exercise
- Physical inactivity
- Alcoholism
- Stress
- Caffeine intake
- Low stomach acid
- Irregular sleep patterns
- High protein diet
- Lack of natural sunlight
- Poor nutrition
- Malabsorption conditions
#2. Symptoms
Osteoporosis is sometimes thought of as an invisible disease, as it can develop gradually without any obvious symptoms. But there are a few warning signs you should look out for as possible ‘red flags’, which should prompt a visit to your GP.
- Loss of height over time
Although height loss can occur naturally as you get older, it may happen more rapidly in those with osteoporosis. A loss of more than 3cm in height is a sign there may be bone issues.
- A curved spine or stooped posture
This may be due to multiple spinal fractures, which cause a change in the spine’s curvature and may happen so gradually it goes unnoticed.
- Unexplained sudden back pain
This sometimes occurs spontaneously as a result of a simple movement such as picking something up off the floor, causing fractured vertebrae. Sudden and inexplicable back pain should be investigated immediately.
- An easily broken bone
Strong bones should be able to withstand a fall or minor bump. If you are over 50 and fracture a bone due to slipping over or a sudden movement, it’s possible you have weak bones.
#3. Building bone strength
It’s never too early to invest in maintaining your bone health. A poor diet and physical inactivity during the growing years may set the scene for bone health issues and brittle bones in later life.
But osteoporosis is not an inevitable outcome. In some cases there may be a genetic component to osteoporosis risk, but developing healthy lifestyle and dietary habits can have a significant impact on the strength and density of your bones.
It’s worth considering the following changes to decrease your likelihood of developing osteoporosis:
- Start a daily exercise routine – the most effective way to promote bone formation and strength is to take part in regular exercise, such as resistance training, tennis, dancing, yoga and brisk walking.
- Stop smoking – smoking is linked to lower bone mineral density and an elevated risk of fractures, particularly in post-menopausal women.
- Find ways to manage stress – stress has a negative impact on digestion and the production of stress hormones such as cortisol, which increase calcium loss through the urine. Meditation, tai chi and yoga are just some practices that may be helpful.
- Get out in the sunshine – just ten minutes a day of sunlight exposure will help boost your vitamin D levels.
- Avoid alcohol – moderation is key. Some research shows that drinking more than three glasses of wine a day has a detrimental effect on bone mass. (5)
#4. The bare bones of nutrition
Strong, healthy bones are bolstered by good nutrition. When planning your meals try to avoid refined carbohydrates, eat less meat and more beans and pulses, include regular portions of oily fish, nuts and seeds, fill your plate with colourful veggies and drink plenty of fluids, preferably water, herbal teas and decaffeinated drinks.
For added peace of mind, the following nutrients should be incorporated into your healthy eating plan:
- Calcium
Calcium is the most abundant mineral in the body and is essential for bone health.
A deficiency of calcium can lead to softening of the bones in adults, and in the long term can contribute to the development of osteopenia, which leads to osteoporosis.
Children with a calcium deficiency are in danger of bone deformities and growth retardation.
Contrary to popular belief, dairy products such as milk, cheese and yogurt are not the only, or best, sources of calcium. The rate of calcium absorption from kale is superior to that of milk. Other dietary sources include tofu, beans, dried apricots, broccoli, nuts, seeds and tinned fish with edible bones such as sardines, and salmon.
If you have trouble obtaining adequate calcium from food, supplementation may be beneficial. Calcium supplements are normally chelated (bonded) to other substances such as inorganic minerals, organic substances or amino acids.
The substance calcium is bonded to determines how well it is absorbed. Inorganic chelates such as oxides, sulphates, phosphates, chlorides and carbonates tend to be cheaper than organic chelates but less well absorbed, necessitating higher doses.
- Vitamin D
Calcium is not the only bone supportive nutrient, vitamin D is also extremely important.
Over a billion people worldwide are deficient in vitamin D, a vital nutrient, known for its ability to stimulate the absorption of calcium into bone tissue.
As humans, we can produce vitamin D in our bodies by the action of sunlight on the skin. However, sunlight deprivation and a lack of vitamin D and calcium in the diet can lead to poor bone health as well as contributing to the development of other chronic health conditions.
Research suggests low levels of vitamin D are linked to the onset of diabetes. (3)
It can be difficult to obtain sufficient vitamin D from food, but there some foods contain adequate levels:
- Fortified foods such as orange juice, milk, yoghurt and breakfast cereals
- Fatty foods like salmon and mackerel
- Cod liver oil
- Eggs
- Beef liver
In terms of bone health, not all types of vitamin D are as beneficial, so if you are considering supporting your diet with supplements, it is advisable to source a vitamin D with high bioavailability. For example, research shows that vitamin D3 is more effective at improving vitamin D status than vitamin D2. (4)
- Vitamin K
Bone mineral density decreases drastically after the menopause, leaving post-menopausal women at greater risk of bone fractures, so much so that over 200 million women worldwide are affected by osteoporosis. Research indicates that post-menopausal bone mineral loss is linked to low levels of vitamin K. (6)
Vitamin K has several different forms, but vitamin K1 and K2 are the naturally occurring forms. It is a fat-soluble vitamin, necessary for the functions of numerous proteins within the body, including osteocalcin, a bone-forming protein.
Vitamin K1 is mainly found in green leafy vegetables, soybean oil and olive oil, and vitamin K2 can be found in small amounts in cheese, egg yolks, chicken and fermented soy beans.
According to research, subclinical vitamin K deficiency is not uncommon. (7) Where dietary levels are poor, supplementing with vitamin K may have therapeutic potential. Studies show vitamin K supplementation reduces bone turnover and improves bone strength.
- Magnesium
Due to an increasing body of evidence, magnesium is now recognised as an important contributor to bone health.
Research suggests that magnesium deficiency contributes to osteoporosis directly, by acting on crystal formation and bone cells. (9)
In one study involving Israeli women, it was found that supplementing with 250mg magnesium daily significantly increased their bone mineral density, compared to the control group who took none. (8)
You can top up your magnesium levels by including brown rice, beans, peas, lentils, nuts and potato skins in your weekly eating plan.
If you suffer from osteoporosis, or are concerned about your bone health, and would like nutrition and lifestyle guidance to help you achieve your health goals, a consultation with an Amchara Personalised Health practitioner can be beneficial.
Why not take advantage of a complimentary consultation today?
Read this next: