According to Arthritis Research UK, arthritis is the biggest cause of pain and disability in this country, with more than a third of people over 45 in the UK seeking medical help for arthritis. (1)
But what exactly is arthritis?
We always take an evidence-based approach and in this article we discuss the main types of arthritis, how they affect sufferers and the treatments that are available, both orthodox and complementary.
Table Of Contents
- Types of arthritis
- Cause of arthritis
- Rheumatoid arthritis versus osteoarthritis
- Gout
- Ankylosing Spondylitis
- Psoriatic arthritis
- How Is arthritis treated?
- Alternative arthritis treatments
- Supportive nutrients
- Positive food choices
- Lifestyle advice
Types Of Arthritis
Arthritis is an umbrella term to describe a variety of musculoskeletal conditions, which cause pain, inflammation and limited movement of the joints surrounding ligaments, tendons or cartilage.
Joints are places in the body where bones come together, such as the hips, knees, toes, wrists and fingers.
Arthritis can affect any part of the body and symptoms vary, depending on the specific type of arthritis.
Arthritis falls into two main categories:
- Inflammatory arthritis – includes conditions such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, systemic lupus and juvenile idiopathic arthritis. (3)
- Non-inflammatory arthritis – includes osteoarthritis.
Evidence suggests that there are more than 100 different forms of arthritis and related diseases. (2)
All of them cause pain in different ways however, some are more common than others, which we will look at in more detail later.
These include:
- Osteoarthritis
- Rheumatoid arthritis
- Ankylosing spondylitis
- Gout
- Psoriatic arthritis
Cause Of Arthritis
Arthritis is generally recognised and diagnosed because of acute or chronic pain, stiffness and inflammation around a joint, often accompanied by structural changes.
Specific causes are as yet unknown, although it is thought that arthritic conditions may be triggered by various factors including crystal deposits in the joints, infection, injury, genetic influences and repetitive use.
Progression of the disease varies depending on the type of arthritic condition suffered.
Rheumatoid arthritis and osteoarthritis are probably the most well known of the arthritic conditions, so we’ll start by discussing the differences between them, the symptoms you might experience and the types of treatment available.
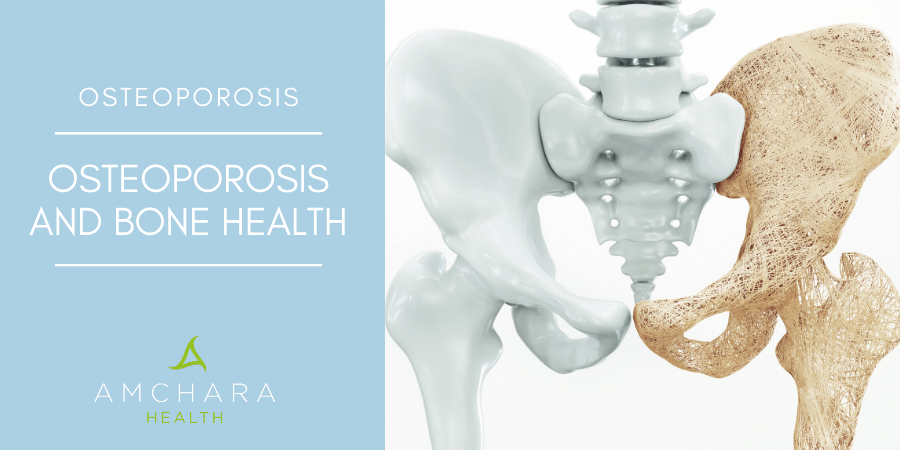
Rheumatoid Arthritis Versus Osteoarthritis
Osteoarthritis is far more common than rheumatoid arthritis and affects around ten times as many people.
Whilst both conditions are forms or arthritis, they have very different characteristics and need different types of treatment.
Osteoarthritis is more common as we age and is often referred to as “wear and tear” or degenerative joint disease, whereas rheumatoid arthritis can occur at any stage of life.
Osteoarthritis is often associated with factors such as injury, ageing and obesity and mostly affects weight bearing joints such as the hands, spine, knees and hips. (4)
Usually, osteoarthritis is a condition that develops very slowly over many years but it can occur at a younger age because of certain repetitive activities, such as typing or running on a regular basis.
But rheumatoid arthritis typically comes on very rapidly and can suddenly develop over weeks or months, rather than years.
Osteoarthritis is categorised as a non-inflammatory form of arthritis, so although the joints may ache and feel slightly painful, initially they are not inflamed or swollen.
However, in more recent years researchers have recognised that over time inflammation does occur as a result of cartilage damage in the joints. (19)
Rheumatoid arthritis on the other hand occurs wholly as a result of systemic inflammation.
Osteoarthritis develops when cartilage that covers the ends of bones in the joints deteriorates.
This is followed by hardening of the joints due to calcification and bone spur formation.
The joint ‘cushion’ deteriorates, causing pain and loss of movement as bone begins to rub against bone.
Over time this can lead to inflammation and loss of cartilage.
Rheumatoid arthritis primarily affects the synovial tissue (the membranes around the joints that secrete lubricating fluid to allow bones to move easily against each other).
It often causes swelling in pairs of joints, especially smaller joints such as the ankles and hands.
However, the entire body can be affected by rheumatoid arthritis, including the heart, lungs and eyes.
People with rheumatoid arthritis may experience systemic symptoms such as:
- chronic fatigue
- low grade fever
- loss of energy
- joint stiffness
- painful swollen joints
- weight loss
- pleurisy
- eye inflammation
- decreased range of motion
Symptoms are generally worse in the morning or after long periods of inactivity.
On the other hand, osteoarthritis sufferers will only experience symptoms in their joints.
Unlike osteoarthritis, rheumatoid arthritis is considered an autoimmune disease and women are more often affected than men.
The disease occurs when the body releases enzymes that attack its own healthy tissue causing the joints to become tender, swollen and sometimes deformed. (5)
Gout
This type of arthritis is very common and was once known as the disease of kings because of its association with a meat and alcohol rich diet.
It is caused when uric acid crystals build up in the joints.
Uric acid is a byproduct of purine metabolism, an organic compound which is either found in foods or made in the body.
Purine rich foods include:
- red meat
- organ meat
- bacon
- alcohol
- anchovies
- sardines
- scallops
- trout
- tuna
- mussels
- herrings
Around one in 40 people is affected by gout in the UK (7) and a large percentage of sufferers are men over 40 or obese adults. (9)
Gout is very, very painful – attacks generally occur at night and often the first occurrence will affect the joint of the big toe.
It usually flares up in one joint at a time.
Signs and symptoms of gout include:
- severe pain in the first joint of the big toe
- fever/chills
- heart and or kidney problems
- constipation
- indigestion
- headaches
Possible causes:
- poor diet
- obesity
- high blood pressure
- metabolic or renal issues that increase production of uric acid or decrease excretion
- chronic anaemia causes increased production of purines
- certain medications that decrease water content of body and increase uric acid levels
- lead toxicity
- stress
Ankylosing Spondylitis
Ankylosing spondylitis is an inflammatory condition primarily affecting the spine, although other joints can be affected.
It causes inflammation in the vertebrae that can lead to severe, chronic pain.
If left untreated, it can result in some of the joints in the spine fusing together.
This makes the spine less flexible, which affects posture and may also cause difficulty with breathing.
Ankylosing spondylitis can affect other areas of the body such as:
- shoulders
- hips
- ribs
- heels
- small joints of the hands and feet
- eyes
- lungs & heart (although rarely)
Possible causes:
The exact cause is still unknown, although genetics are thought to be a major factor in the disease.
It is also believed that ankylosing spondylitis may start when the intestinal barrier breaks down and pathogenic bacteria pass into the blood circulation – triggering changes in the immune response.
Psoriatic Arthritis
This is another form of arthritis considered an autoimmune disease, whereby the body’s own immune system runs out of control and attacks normal tissues in the body.
According to the NHS up to two in every five people who suffer from psoriasis will go on to develop psoriatic arthritis. (10)
Signs and symptoms :
- swelling in the joints
- swelling in tissue surrounding the joints
- stiffness
- red patches of skin
- silvery scales
- joint pain
- changes in the nails
- extreme fatigue
Psoriatic arthritis can affect other parts of the body including the spine, elbows, neck, feet and fingertips.
Flare ups can be unpredictable and varying in severity.
Psoriatic arthritis is a long-term condition that can gradually worsen leading to permanent joint damage and deformity that may require surgical treatment. (10)
Diagnosing arthritic conditions that are autoimmune in nature is usually via simple blood tests.
How Is Arthritis Treated?
Conventional treatment for arthritic conditions generally involves the use of nonsteroidal anti-inflammatory drugs (NSAIDs), steroids and painkillers.
Uric acid lowering drugs are also prescribed for gout. (8)
These medications are usually recommended because they are highly effective at relieving many of the symptoms of arthritis – however, they have little effect at reducing the progression of arthritis.
Drugs of this kind need to be taken regularly and usually long term to gain the benefits.
Unfortunately, such drugs are not without unwanted side effects and many patients experience gastric pain or diarrhoea, due to irritation of the stomach.
Damage to the gastro-intestinal tract may increase the risk of ulcers. Chronic use can also accelerate joint destruction and lead to kidney problems.
It should be noted that although NSAIDs prevent prostaglandin formation in order to decrease inflammation, they also inhibit cartilage synthesis and increase cartilage destruction, which is why they may actually accelerate osteoarthritic progression. (6)
As osteoarthritis is considered a non-inflammatory form of arthritis, the treatment is a little different.
Conventional GPs will usually recommend dietary and lifestyle changes, including exercise and changes in food choices.
Mobility and activity are key approaches to managing symptoms.
GPs are also likely to recommend painkillers to reduce pain and inflammation in the joints, which carry similar risks to the drugs diagnosed for rheumatoid arthritis.
Bearing in mind the potential for adverse side effects, taking medications in the long term is not everyone’s preferred course of action, so it makes sense to consider alternative approaches to managing the uncomfortable symptoms associated with arthritic conditions.
Alternative Arthritis Treatments
Many things can be done to reduce the impact of arthritis on everyday life.
The key is early diagnosis and a treatment plan tailored to the needs of the individual.
Therapy should include healthy nutrition, regular and appropriate exercise, weight control, manipulation, use of heat and cold, and supplementation.
As with many other degenerative or autoimmune disorders, poor nutrition is often the major detrimental influence.
It is common to find that many individuals suffering from arthritis have dietary patterns that are not ideal.
As well as following some of the nutrition guidelines suggested below, the question of food intolerance should also be investigated, especially in rheumatoid arthritis.
Some of the foods cited as culprits that can aggravate arthritis symptoms include:
- dairy products
- soya
- wheat
- nightshade family (potato, peppers, aubergines, tomatoes and tobacco)
These foods contain a toxin called solanine, which in certain sensitive individuals needs to be avoided, particularly those suffering with arthritis.
This toxin is thought to interfere with enzymes that increase the levels of neurotransmitters, causing prolonged muscle contractions, pain, tenderness and inflammation. (15)
A standard elimination diet is the best way to identify problematic foods but should only be followed under the guidance of a qualified Health Practitioner.
As much of the pain and discomfort in arthritic conditions is due to underlying inflammation within the body, managing inflammation effectively may make the joints more comfortable.
Supportive Nutrients
The first approach should always be the diet.
There are a number of nutrients with natural anti-inflammatory properties that may be especially helpful, regardless of the type of arthritis you are suffering from.
Antioxidants are produced by the body to protect you from substances such as free radicals than can damage cells and tissues.
Excessive and inappropriate production of these pro-oxidant compounds is associated with inflammatory disease.
Antioxidants are found in a range of foods but especially in fruit and vegetables.
Bromelain is a digestive enzyme found in pineapples. Normally, when taken with food it aids digestion, however if taken away from food it has anti-inflammatory properties.
Devil’s Claw is an herbal remedy native to Southern Africa. It contains constituents within the roots called harpagosides, thought to reduce pain, stiffness and symptoms of osteoarthritis, as well as increasing physical function.
Ginger suppresses pro-inflammatory prostaglandins, the chemicals our body produces from essential fats.
Omega-3 essential fatty acids help to suppress pro-inflammatory cytokines, or cell signalling chemicals.
Quercetin is thought to have anti-inflammatory properties. It is believed to exert its effect by interfering with the production of chemicals, which cause inflammation such as leukotrienes and prostaglandins.
Foods rich in quercitin include apples, broccoli, onions, green tea, spinach, red grapes, tomatoes, berries, parsley and sage.
It should be noted however, that foods can lose their quercitin content when cooked, especially after boiling or if they have been stored for lengthy periods.
Vitamin C is an important factor in collagen synthesis, which is necessary for the formation of cartilage and bone.
In addition to this, some studies have shown that vitamin C significantly altered the levels of uric acid in the blood of patients suffering with gout. (17)
Vitamin D plays a key role in managing inflammation. Several studies have identified that it plays a part in regulating the production of inflammatory molecules (14).
Many people in the UK are deficient in vitamin D, simply because they don’t get enough exposure to the sun.
Research has also identified that those with inflammatory diseases tend to have lower vitamin D status.
During the winter months supplementing may be necessary to ensure adequate vitamin D levels in the body.
Positive Food Choices
Weight control is an important concern for those with arthritis.
Keeping close to your ideal weight helps decrease the pressure on problematic joints such as the hips and knees, which bear much of the weight of the body.
In addition, research has now confirmed that weight loss can prevent the onset of osteoarthritis, relieve symptoms, improve function and increase quality of life. (16)
Maintain balanced blood sugar levels to help with weight management.
Instead of refined sugary foods such as pasta, white bread, biscuits, pastry and cakes, switch to whole grains such as:
- oats
- brown rice
- quinoa
- millet
- bulgur wheat
- vegetables/fruit
An additional benefit of whole grains is they contain plenty of filling fibre, which can help to maintain a healthy weight.
Some studies have also shown that fibre-rich foods help to lower blood levels of the inflammatory marker C-reactive protein. (3)
However, caution may need to be taken with gluten containing grains such as wheat, as the protein gluten has been linked to inflammation for some individuals.
Increasing anti-inflammatory foods is vital for arthritis sufferers.
Regularly include:
- garlic
- turmeric
- ginger
- onions
- watercress
- oily fish: salmon, mackerel, sardines, fresh tuna
- walnuts
- flaxseeds
Eat plenty of fruit and vegetables. As well as being an excellent source of fibre, they are also a rich source of nutrients and antioxidants. Aim for at least five portions a day.
Dark blue and purple coloured berries and grapes are particularly rich in types of flavonoids called anthocyanins and proanthocyanidins. These phytonutrients are very powerful antioxidants and anti-inflammatory agents.
Add fibre and protein to each meal. This helps to keep blood sugar balanced throughout the day. Include nuts, seeds, fish, poultry, eggs, lean meat and tofu.
Reduce red meat consumption. Many meats contain high levels of saturated fat, the type of fat that promotes inflammation. Evidence suggests that red meat is an independent risk factor for arthritis. (13)
Include foods high in omega-3 essential fatty acids. Choose salmon, mackerel, sardines, herrings, fresh tuna, flaxseeds and walnuts.
Reduce or eliminate trans-fatty acids. Mostly found in commercially produced processed foods such as biscuits, crisps, cakes, onion rings, margarine, crackers and chips. These types of foods have been linked to obesity.
Avoid sugars. Particularly fructose found in many processed foods which can promote inflammation and make arthritis worse. (11)(12) Foods that are high in fructose include soft drinks, fruit juices, dried fruit, sweets and shop-bought salad dressings.
Lifestyle advice
Embrace the importance of exercise. Research has highlighted important benefits of exercise, combined with weight management, to reduce arthritic pain.
Moderate, regular exercise can significantly improve mobility and pain but bear in mind that overdoing it at the gym, or working out too late in the evening, may intensify symptoms.
Proper exercises performed on a regular basis can help to decrease fatigue, improve sleep, keep bones and muscles in motion, build muscle strength, increase flexibility and stamina, and improve the general sense of wellbeing.
Research has also found that exercise helps to replenish lubrication to the cartilage of the joints, thus reducing pain and stiffness. (20)
An additional benefit is that exercise can enhance weight loss and promote long-term weight management for individuals with arthritis who are overweight.
It is worth seeking help from a physiotherapist or osteopath, who can design exercises to achieve specific goals, tailored to individual needs.
Recreational exercise, depending on the degree of movement a person can tolerate, may include walking, cycling, swimming, exercise classes or light weight training.
Try baths and massages. Soaking in a warm bath with Epsom salts may help to relax the muscles and remove toxins from the joints.
Apply warm or cool packs. You may find that the use of heat or cold, or alternating use of the two, lessens stiffness and painful sensations in your limbs.
Apply warming balms containing ginger, eucalyptus and aloe vera.
Try more cooling balms if there is a lot of heat in the joints. Products that contain menthol are particularly helpful.
Visit an osteopath for musculoskeletal support. Osteopathy is a discipline concerned with the musculoskeletal system, the bones, joints, muscles, ligaments and connective tissue and its relationship with the body as a whole.
Practitioners will use physical manipulation to treat a variety of ailments, including arthritis.
Try Acupuncture, practiced in China for more than 3,000 years and now widely recognised and used in the UK.
Acupuncturists restore the flow of body energy – called Qi – by stimulating certain points on the body either by inserting small needles in any one of over 400 acupuncture points or applying massage.
Results from a number of studies suggest that acupuncture may help ease a variety of chronic types of pain such as lower back, neck and knee pain, and osteoarthritis. (18)
Takeaway
Trying to manage arthritic symptoms through diet can be challenging, especially if you are unsure whether your diet contains trigger foods.
As mentioned earlier elimination diets can help to identify these but need to be carried out with the support of a qualified Health Practitioner.
Amchara have a team of experienced Health Practitioners who are available to guide you through this process and can offer additional support regarding appropriate supplementation and additional complementary therapies that may be immensely beneficial.
Complimentary consultations are available if you would like to determine the kind of support you need.
Did you find this article useful?
Do you have any other suggestions that have helped you manage arthritis?
READ THIS NEXT: