Mental health issues are one of the worlds leading causes of disability – the World Health Organisation (WHO) estimates that over 300 million people worldwide experience depression.
Symptoms of depression do not only involve persistent low mood but can also involve anxiety, fatigue, brain fog as well as aches and pains.
We always take an evidence-based approach and aim to provide you with actionable knowledge and tips to help you on your journey to optimal health.
In this article, we will discuss how depression is linked with inflammation and how anti-inflammatory foods may help when tackling depression.
Depression and inflammation
Depression is a complex condition and many factors are linked to its development, ranging from imbalances of mood influencing neurotransmitters such as serotonin and dopamine, through to nutritional deficiencies, genetics and life stresses.
For over a decade significant research has focussed on the inflammatory side of depression.
It is not fully known if depression is the cause of inflammation in the body or if the inflammation is leading to depression, but what does appear to be the case is that there is a strong link with high levels of inflammation and symptoms of depression (1).
There is also a high incidence of depression in many inflammatory conditions such as rheumatoid arthritis (2), Crohn’s disease and ulcerative colitis (3).
Inflammation is a natural immune response and occurs when the immune system detects injury, damage or a foreign organism like a bacteria or virus.
The inflammatory response involves many cells, proteins, tissues and messengers and is responsible for ‘marking’ damaged tissue or pathogens, allowing the rest of the immune system to recognise and remove the problem.
Inflammation is a necessary part of the removal of debris, toxins and the healing process.
Although most commonly thought of as a localised response (think of an injured ankle swelling up and becoming hot and red), inflammation can become chronic and involve the whole body.
This low-grade systemic inflammation leads to increases in inflammatory markers such as ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) which can be detected by a blood test.
Common symptoms experienced in chronic inflammation may include fatigue, headaches, muscle stiffness or aches and a general feeling of ‘coming down with something’.
How inflammation affects mood
During the inflammatory process messengers called cytokines are released – they are a crucial part of the process of sending signals to immune cells and directing the immune response.
There are many different types of cytokines and they may have anti-inflammatory actions or they may actively promote inflammation.
In depression, there is a rise in cytokines that increase inflammation (1,4,5).
The mechanism behind how inflammation may influence mood is not fully understood but it is thought that the actions of certain cytokines may influence the production of the mood neurotransmitter serotonin.
Serotonin production is under the influence of several nutrients and enzymes.
The amino acid tryptophan is used in the body for serotonin synthesis.
Certain inflammatory cytokines have been shown to increase the activity of an enzyme, called IDO, that can send tryptophan down a non-serotonin pathway that can create potentially neurotoxic molecules (6,7).
This limits serotonin production which may affect mood.
Causes of inflammation
There are many sources of inflammation – exposure to several factors that contribute to low levels of inflammation may actually be fuelling chronic low grade systemic inflammation.
- Food
Food contains a variety of vitamins, minerals, amino acids, fatty acids and plant phytochemicals that all work together to support health and vitality.
During processing and manufacturing some of these essential nutrients may be damaged, removed or altered, leading to an imbalance and usually something that is far from the original food.
Think of white, refined flours – the husk and the bran (and therefore the beneficial nutrients) are stripped out and manufacturers are legally obliged to fortify the end product as it is nutritionally inadequate.
Eating a diet high in refined, processed foods, sugars and saturated or trans fats has been shown to be linked to inflammation (8).
Trans fats are formed during the processing of vegetable oils (hydrogenation) and are found in snack foods, pastries, packaged baked goods and margarines.
Food allergies, intolerances and sensitivities may also play a role as the immune system mounts a response to what it sees as a ‘foreign’ food and levels of inflammation rise.
Gluten containing grains like wheat, rye, barley and spelt are known to cause inflammation in the gut (9) and for some people may cause significant damage to the gut lining.
The gut lining acts as a natural barrier to prevent the entry of undigested food particles, foreign molecules or bacteria into the blood stream.
When this natural barrier becomes damaged or ‘leaky’ it allows entry of particles that the immune system reacts to and therefore leads to increased inflammation.
- Microbiome balance
The complex eco-system that resides in the gut, called the microbiome, exerts many functions in the body, and not only communicates with the brain and influences neurotransmitter levels, but also plays a role in inflammation.
An imbalance of the types, or numbers of organisms naturally resident in the gut, also called dysbiosis, may negatively affect the inflammatory process.
There are many factors that can cause disruption to the microbiome and these include poor food choices, stress, lack of sleep, chemicals and the use of medication – particularly antibiotics.
- Infection
The immune system is well armed to deal with infections from bacteria or viruses and, as we know, the inflammatory response is part of detecting and eradicating any infections.
In normal circumstances, once the pathogen has been dealt with, the immune system settles down and levels of inflammation should drop.
However, there are a number of viruses or other pathogens that may lay dormant in the body and contribute to long term low grade increases in inflammation.
Symptoms of depression may be seen alongside an increase in inflammatory markers in dormant viral infections, such as Epstein-Barr, herpes simplex and cytomegalovirus (10).
Even the flu virus has been linked to symptoms of depression and anxiety (11).
- Obesity
Statistics indicate that around 62% of people in the UK are obese.
Fat cells are known to increase pro-inflammatory factors and suppress anti-inflammatory factors (12), and an increase in body fat may well be fuelling the fire when it comes to inflammation.
Obesity may well be the most common source of low grade inflammation.
- Lifestyle
Stress and depression often come hand in hand during times of high psychological stress hormones such as cortisol are released.
Initially, cortisol has anti-inflammatory actions but over time the prolonged exposure to cortisol, as in chronic stress, creates a resistance to the actions of cortisol. Cells become ‘deaf’ to the anti-inflammatory actions and inflammation is allowed to continue (13).
Sleep disorders affect around a quarter of people in the UK and can affect quality of daily living as well as having impacts on long term health.
A lack of sleep is known to contribute to poor mood, but insomnia can contribute to the development of mental health disorders.
A reduction in sleep duration, even only by 2 hours a night, may raise pro-inflammatory cytokines (14).
A lack of physical activity also negatively impacts overall levels of inflammation, and leading a sedentary lifestyle has detrimental effects on health outcomes.
Increased inflammation may be reversed through increasing physical activity (15).
Nutrition and depression
It is important to understand the role of food in mood, as many foods provide nutrients that are necessary for the healthy production and breakdown of mood influencing neurotransmitters.
The importance of the right foods for good mental health has been the focus of the Food for the Brain charity for many years.
Neurotransmitters that influence mood are produced from amino acids.
Serotonin, the happy neurotransmitter, is made from tryptophan.
Protein rich foods like organic grass fed poultry, beef, tuna, salmon, tofu and tempeh contain tryptophan and seeds like chia and flax also contribute to levels.
Dopamine is a neurotransmitter that assists with mood, motivation and pleasure and can also be found in the same foods that are rich in tryptophan, as well as eggs, pumpkin seeds and beans.
In order for the amino acids to be converted to neurotransmitters, several co-factors are required.
These assist enzymes to function correctly, and if there is a lack of a co-factor conversion may be impaired.
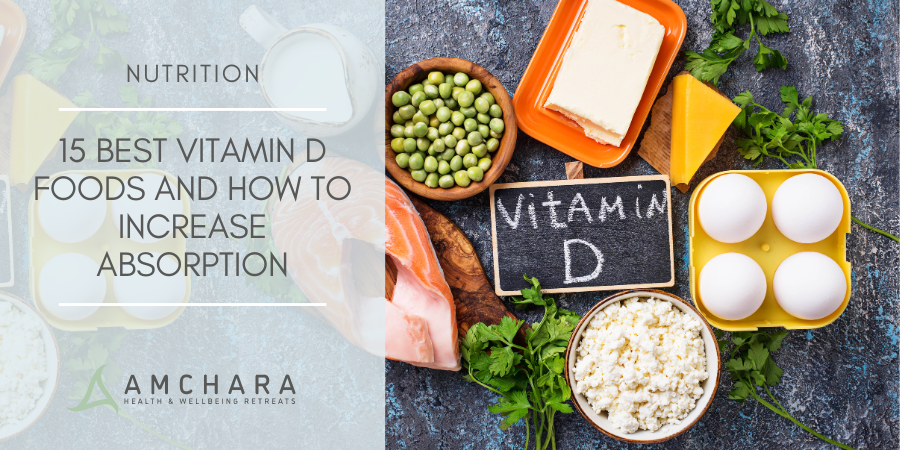
The minerals iron and zinc and vitamin B6 all play vital roles in neurotransmitter synthesis.
Foods rich in iron include:
- organic grass fed animal proteins
- eggs and spinach
- dried apricots
Zinc is high in shellfish, organic grass fed meat and pumpkin seeds.
A good intake of vitamin B6 may be obtained by eating salmon, tofu and bananas regularly.
Folate and vitamin B12 are essential for a cycle in the body that is responsible for the healthy production and breakdown of neurotransmitters.
Alterations to levels of either of these nutrients can give rise to symptoms of depression.
Vitamin B12 is found in good levels in animal proteins, and folate can be obtained from dark green leafy vegetables including asparagus, spinach, broccoli and avocado.
When it comes to a specific diet and the reduction of depression, several studies indicate that the Mediterranean diet is one of the most beneficial.
It is classed as an anti-inflammatory diet and includes whole foods, fruits, nuts, vegetables, legumes, cereals, olive oil, oily fish, and a low meat and dairy consumption.
A moderate alcohol intake is also common.
Altering the types of foods eaten and increasing foods that have a natural anti-inflammatory action may be useful for tackling depression.
Anti-inflammatory foods for depression
- Oily fish
Fatty fish such as salmon, herring, trout, sardines, mackerel and pilchards are not only good protein sources but also contain omega-3 fatty acids.
These are essential fatty acids that cannot be made in the body and so a good dietary intake is needed.
The omega-3 fats are used in the body to make anti-inflammatory molecules and a good intake has positive effects on mood (16).
Eating 2-3 portions of oily fish a week and including seeds such as flax seeds and chia seeds and walnuts also contributes to levels.
Keeping omega-6 rich foods in balance is also a key step as too much omega-6 in the diet can prevent omega-3 from being used effectively.
Highly processed foods, ready meals, take aways, vegetable oils and margarines are often high in omega-6 and should be reduced. Eating organic grass fed meat and poultry provides a better omega-3 to -6 balance.
- Fruit and vegetables
Rich in many vitamins, minerals and phytonutrients, there are many benefits to increasing fruit and vegetable intake.
Some of the most potent plant nutrients can help to regulate the immune system and keep inflammation in check.
The wide variety of colours to fruits and vegetables comes from the antioxidants that they contain.
These antioxidants help to ‘mop up’ damage in the body and many antioxidants work better together than alone.
Some important antioxidants include carotenoids, vitamin E, vitamin C and polyphenols such as flavonoids.
It is important to eat as wide a variety as possible, to provide a good balance of all types of beneficial nutrients.
Aim to eat all the colours of the rainbow and try to include red, orange, yellow, white, green, blue and purple fruits and vegetables daily.
An optimal intake is around 8-10 portions a day with more vegetables than fruit. Using a rainbow food wheel can be a useful way to track daily intake.
Colour
Food
RED
Tomatoes, red peppers, radish, rhubarb, cranberries, goji berries,
raspberries, strawberries, watermelon, red apple, cherries,
pomegranates, red cabbage, red onion, plum, pomegranate, radicchio
ORANGE
Carrots, squash, pumpkin, orange peppers, apricot, sweet potato,
mango, papaya, nectarine, oranges, tangerines
YELLOW
Grapefruit, lemons, pineapple, cantaloupe, banana,
summer squash, yellow peppers,
WHITE-
TAN
Apple, cauliflower, mushrooms, onions, pears, turnips,
fennel, parsnips, white peaches, coconut,
Jerusalem artichoke, nuts, seeds
GREEN
Apples, artichokes, asparagus, avocado, celery, rocket, watercress,
spinach, kale, spring greens, broccoli, green peppers, green beans,
cabbage, Bok Choy, Brussels, lettuce, okra, peas, swiss chard,
cucumber, sugar snap peas, kiwi, courgette, olives, rosemary,
parsley, coriander
BLUE-
PURPLE
Blueberries, blackberries, blackcurrants, olives, purple carrots,
beetroot, aubergine, purple broccoli, black grapes, elderberries, figs
Fruit and vegetable intake can be increased by ensuring half your plate at lunch and dinner is made up of vegetables. Juices, smoothies and soups are also handy ways to increase your daily intake.
Lightly steaming vegetables ensures they retain the water soluble nutrients.
Some nutrients are better when combined with an oil such as lycopene in tomatoes and some of the carotenoids.
In fact, one interesting study showed that adding avocado, or avocado oil, to a salad can significantly increase carotenoid absorption (17).
- Spices
Not only do spices add a depth of flavour to food, but they can also bring health benefits.
Many spices have anti-inflammatory properties, and some are particularly useful when it comes to mood.
Turmeric contains curcumin which gives turmeric its bright yellow-orange colour. It has potent anti-inflammatory properties and shows great benefit in relieving depression (18).
It can be a great addition to curries, helps to liven up roasted vegetables and can be added to warm milk to make a traditional Ayurvedic drink called golden milk. Turmeric tea is also another way to increase intake.
Be sure to add a fat like coconut oil when using turmeric as curcumin is fat soluble and therefore fat enhances absorption. Combining turmeric with black pepper also enhances its bioavailability.
Ginger is another tasty anti-inflammatory spice and is a great addition to carrot and beetroot juice. It lends itself well to stir fries and curries as well as other Asian dishes.
- Olive oil
One of the key components of a Mediterranean diet, olive oil is rich in an omega-9 fatty acid called oleic acid. Regular consumption of olives and olive oil has been shown to reduce the risk of depression as well as inflammation (19).
- Green tea
A common drink in Eastern cultures, green tea is showing many health benefits.
It has potent antioxidant compounds such as epigallocatechin gallate (EGCG) and a higher intake of green tea is associated with lower incidence of depression (20).
It is also rich in an amino acid called theanine, which promotes calming alpha brain waves, usually seen in deep states of relaxation (21).
- Fermented foods
Traditional and Asian fermented foods such as kefir, kombucha, kimchi, kvass, sauerkraut, tempeh and miso are good sources of beneficial probiotic bacteria.
As the microbiome exerts a balancing effect on the immune system – and imbalances in gut bacterial balance may favour inflammation – including fermented foods regularly may positively affect levels of inflammation and mental health (22).
- Keep inflammatory foods low
It should go without saying that if you wish to reduce inflammation then avoiding or reducing foods that cause inflammation in the body is key.
Foods linked to inflammation include:
- Sugar
- Gluten containing grains
- Processed and packaged foods
- Trans fats
- Excess alcohol
- Fried and charred foods
- Processed red meats like sausages, ham, bacon and salami
- Dairy
Depression involves many factors, and it is evident that chronic inflammation is often present.
Making nutritional changes to reduce inflammation may be a key step in tackling depression.
Getting further support and advice from a Personalised Health practitioner experienced in mental health can help you to investigate other factors that may be playing a role.
We are always interested to hear about your own personal experiences, what have you found helps to improve your mood?
Have you tried an anti-inflammatory approach?
Sharing experience and knowledge helps to support others, please leave your comments below.
READ THIS NEXT: